Table Of Contents
- 1 The baseline: how often do implants fail?
- 2 Why nicotine derails healing
- 3 Vaping: not a harmless workaround
- 4 How long should you quit before and after surgery?
- 5 The hidden financial upside
- 6 Tactics that help the quit stick
- 7 What about light or social smokers?
- 8 Key take-home
- 9 Frequently Asked Questions
Dental implants are among the most predictable procedures in modern dentistry, yet even the best-planned surgery can come unstuck when nicotine enters the picture. This article unpacks the evidence behind smoking, vaping and implant survival, and offers clear timing advice for quitting that applies whether you are booking a single crown or full mouth dental implants Melbourne.
The baseline: how often do implants fail?

Large cohort studies report an overall failure rate of roughly 5 – 7 % in healthy non-smokers. Smokers, however, see that figure creep far higher. A 2020 systematic review found the risk of implant loss more than doubles for people who smoke more than a pack a day (relative risk 2.45 on an implant level; 4.0 on a patient level) Ten-year follow-up research echoes the trend: survival sat at 94.2 % for non-smokers versus 85.5 % for smokers. Another pooled analysis of over 6 000 fixtures reported an 8.3 % failure rate in smokers against 4.3 % in non-smokers.
These numbers matter if you are weighing up teeth implants cost Melbourne, because revision surgery demands extra chair time, new components and often bone grafting. Put simply, nicotine burns a hole in more than your pocket.
Why nicotine derails healing
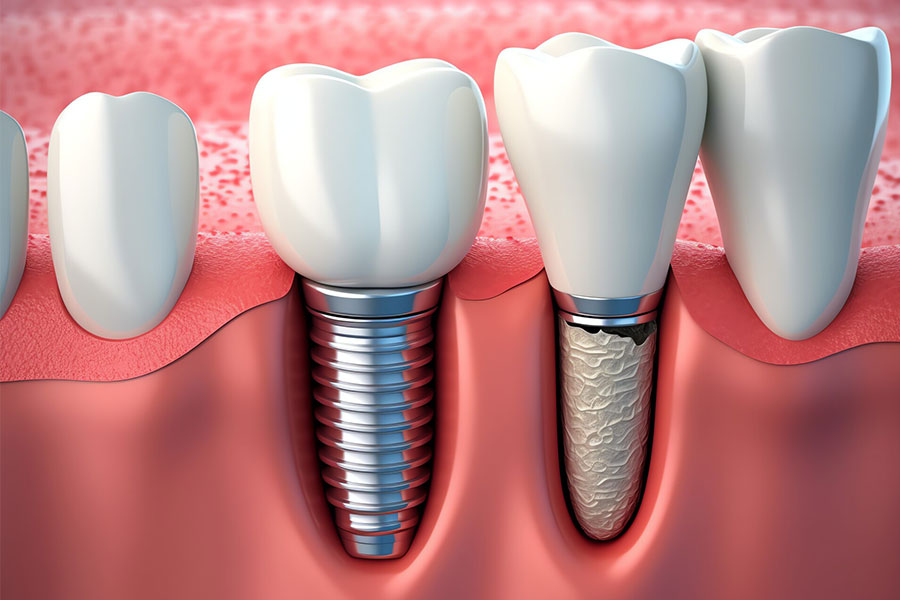
Osseointegration—the intimate contact between titanium and bone—relies on a well-orchestrated dance of blood flow, osteoblast activity and immune balance. Nicotine interrupts every step. Laboratory work shows it lowers osteoblast numbers while boosting bone-resorbing cells, reducing the very scaffold an implant needs to lock in place. Restricted capillary blood flow and thicker platelets further starve the surgical site of oxygen. The end result is slower bone formation, a higher chance of early micro-movement and, ultimately, loss of stability.
Vaping: not a harmless workaround
Many patients assume that swapping cigarettes for e-cigarettes solves the problem. The data suggest caution. Emerging clinical studies link e-cigarette aerosols to peri-implant inflammation and crestal bone loss comparable to, and in some cases worse than, conventional smoking. If your goal is long-term implant success, vaping is not a loophole.
How long should you quit before and after surgery?
Guidelines vary, so let’s translate them into a timeline you can actually follow:
| Quit window | Practical tip |
| At least 1 week before and 2 months after | Mark the surgery date on a calendar and block off ten weeks smoke-free. |
| Six weeks nicotine-free before placement | Use nicotine-replacement therapy that avoids the gum or implant site. |
| Minimum 12 hours before surgery | Applies if you are unable to quit earlier—still better than lighting up on the day. |
Quitting earlier is always better. The bone-forming cycle around an implant continues for months, so staying smoke-free beyond the initial eight-week window protects against late complications such as peri-implantitis. If abstinence feels daunting, ask your GP about prescription aids; Australia’s PBS covers several options.
A failed fixture means more imaging, more surgical kits and often a custom abutment remake. Re-scheduling theatre time in a busy city centre clinic drives the bill up rapidly. Patients who search “dental implants near me prices” often focus on the headline figure, yet the true cost of a smoking-related failure can double the outlay. By contrast, those who stop smoking early not only keep the original implant but also gain better gum health—saving on hygiene maintenance down the track.
Tactics that help the quit stick
- Set a firm date: pick a quitting day at least six weeks out from surgery and tell your dentist; accountability matters.
- Replace the ritual, not just the nicotine: swap coffee-and-cigarette breaks for a brisk walk or herbal tea.
- Use guided apps: several Australian government-endorsed apps provide daily check-ins and cost-savings trackers.
- Consider combination therapy: a patch for baseline control plus an inhalator or lozenge for cravings gives the highest success rates, minus oral soft-tissue irritation.
- Follow-up: schedule a review call one week post-placement when temptation peaks.
These steps turn the stats in your favour and make any search for dental implants near me affordable more meaningful—because affordable only counts when the implant lasts.
Even low-frequency smoking raises failure risk. The systematic review noted earlier found that the dose-response curve is steepest in the first ten cigarettes per day, then plateaus. Put plainly, there is no safe threshold. If you smoke at weddings or on Friday nights, have an honest chat with your surgeon. Full disclosure lets the team tailor postoperative care, such as extended antibiotic courses or extra hygiene visits.
Key take-home
- Nicotine—whether burnt or vapourised—roughly doubles the odds of implant failure.
- Aim for at least one smoke-free week before surgery and eight weeks after; six weeks pre-op is even better.
- Vaping is not risk-free and should be paused under the same timetable.
- Protect your investment: the average cost of a single implant crown in inner-city clinics rivals two overseas holidays; imagine repeating that because of a cigarette.
- If you are shopping for dental implants Melbourne, ask the clinic about their smoking protocol and support resources.
Choosing to quit is the single most effective way to protect your new tooth. That decision, coupled with a skilled surgical team, turns a statistic into a success story. When you finally run that local search for dental implants near me, make sure the result leads to a smoke-free, long-lasting smile.
Frequently Asked Questions
1. How does cigarette smoke affect osseointegration of dental implants?
Smoking constricts blood vessels, reduces oxygen tension, impairs osteoblast function and encourages bacterial colonisation around the fixture. Together those factors slow bone formation and increase micromovement, doubling the likelihood of early implant loss compared with non-smokers, according to studies.
2. Is vaping safer than smoking when planning dental implants?
Evidence says no. Vapour contains radicals, aldehydes and metals that inflame peri-implant tissue and erode bone. Clinical studies show survival matching or sometimes trailing smokers. Accordingly, clinicians urge complete nicotine abstinence during the critical pre- and post-operative healing period.
3. What smoke-free period do experts suggest around implant surgery?
Surgeons recommend quitting one week before placement and staying nicotine-free eight weeks afterwards, the window when new bone anchors titanium. Extending to six weeks pre-op further lowers failure risk. These guidelines cover cigarettes, e-cigarettes, cigars and smokeless products alike.
4. May I use nicotine-replacement therapy while my implant heals?
Yes. Patches, gum, lozenges and inhalators deliver nicotine without the carbon monoxide and tar that hamper blood flow. Patches are preferred because they avoid oral contact, reducing irritation. Discuss the dose carefully with a GP or pharmacist before surgery.
5. What signs suggest my implant site is suffering after a smoking relapse?
Watch for swelling, bleeding gums, foul taste, and tenderness when tapping the crown. Early X-rays may show crestal bone loss. Contact your dentist immediately; prompt debridement and antimicrobials can salvage a compromised implant before mobility develops.

